Access to behavioral health care services remains a critical need for Massachusetts residents. Even when accessible, care is often fragmented between behavioral and physical health. Inequities in access to behavioral health care have been exacerbated by stigma and other structural forces such as racism, and those with substance use disorders (SUD) are often socially marginalized. Recent data shows rising rates of opioid-related overdose deaths among Black and Hispanic populations, and disparities in access to treatment for behavioral health conditions and opioid use disorders (OUD).
Behavioral health care services are associated with better health outcomes and more efficient use of health care overall, with better management of behavioral health conditions found to lower overall health care spending and improve quality of life. Despite this, behavioral health care services remain relatively underpaid compared to specialty services. Policymakers across the U.S. have sought to increase access to and funding for behavioral health care for these reasons.
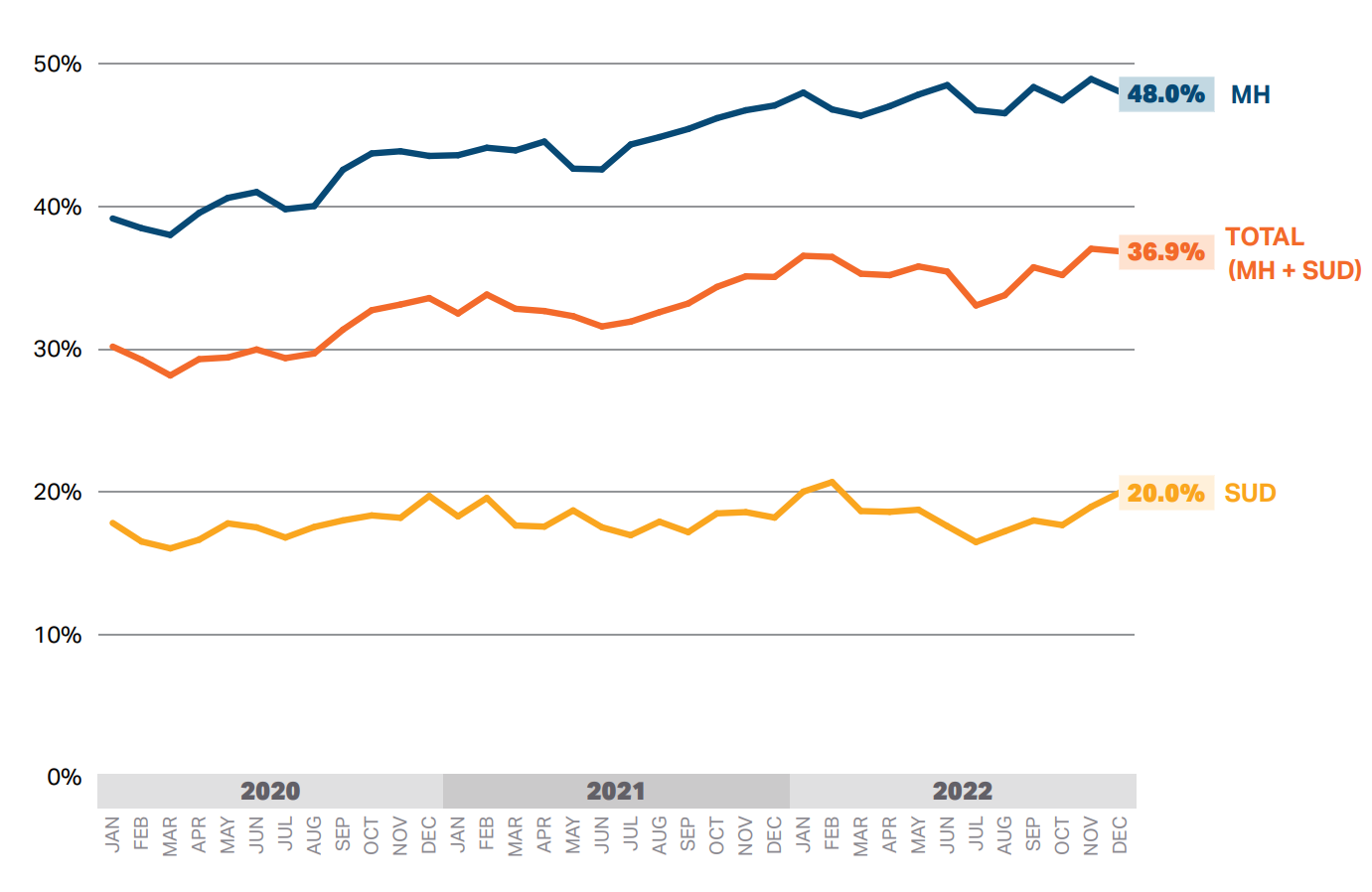
The HPC conducts research to monitor key metrics in the provision of behavioral health care services, including both cost and utilization, as well as the increasing shortages of care providers in the behavioral health workforce and the associated impacts of these challenges. The 2023 Health Care Cost Trends Report includes a new chartpack exploring trends in behavioral health care, including the use of telehealth for psychotherapy services, opioid-related hospitalizations, and other behavioral health-related inpatient stays and emergency department (ED) visits. This research builds on prior HPC research studying behavioral health-related “boarding” in the ED (i.e., patients spending 12 or more hours in the ED from the time of arrival to time of departure), a consequence of inadequate outpatient and inpatient supply of behavioral health care services. The share of behavioral health-related ED visits resulting in boarding grew from 2020 to 2022, driven by an 8.6 percentage point increase in boarding for mental health-related stays.
Percent of behavioral health-related ED visits that resulted in boarding (>12 hours) by type, 2020–2022
Addressing behavioral health needs is a priority embedded into the HPC’s investment program portfolio, either as a core focus or as an important consideration within initiative care models and innovations. Multiple HPC investment programs and awardee initiatives have centered on expanding access to evidence-based, culturally-competent addiction treatment that is free of stigma and bias, including for birthing parents with SUD as well as infants exposed to substances in-utero. These often include connecting patients to cost-effective treatments – particularly Early Intervention and medication for opioid use disorder (MOUD) – that can help improve outcomes. Other awardee initiatives have centered on implementing whole-person care models in community hospitals to integrate care across medical, behavioral health, and social needs, increasing screening and access to behavioral health care services in primary care settings, and using telemedicine to extend access to specific populations with unmet behavioral health needs. Learn more about the HPC’s investment programs, including profiles of specific awardee initiatives and their impacts on patient care.
